5 Guidelines To Get You Started
By Cynthia D. Smith, PharmD
Making good food choices is always important, but especially so when you’re pregnant.
And if you are pregnant and have diabetes, your choices can be crucial to your health and your baby’s health.
What you eat helps regulate your blood sugar and your baby’s. And keeping your blood sugar in a healthy range can help decrease potential problems, now and in the future.
Of course, the best meal plan is one that’s created by your health care provider. He or she will create a plan that has been tailored to your specific needs.
But what should you do if you’re waiting to see your registered dietitian or certified diabetes educator? You’re ready to get started right now, you’re ready to eat healthy, you want to get your blood sugar under control. But how? What do you need to do?
Keep reading.
Below are guidelines to help you get started and a sample menu plan that shows you how it all fits together.
But remember: There may be other special nutritional needs to consider. Are you having twins? Have you had gastric bypass surgery? Are you a vegetarian or have other dietary restrictions? Also, this information is geared toward women with gestational diabetes, not all pregnant women.
It’s only a guide. It does not take the place of your health care provider’s recommendations.
Okay. Enough said. Here are the Gestational Diabetes Meal Planning Guidelines.
#1 Eat 3 Meals and 3 Snacks Every Day
Three meals and three snacks every day! Seems like a lot, doesn’t it? Maybe you have a habit of skipping breakfast, grabbing lunch on the go, then finally at the end of a long day you’re able to sit down and have a decent meal.
Well, it’s time to make some changes.
Instead of waiting for your hunger to build and build until it’s ready to explode, try pacing your meals throughout the day. As a bonus, you’ll be less likely to give in to cravings.
With a little planning and some practice, it will be easier than you think.
A good meal plan consists of three meals and three small snacks eaten about every 2 to 3 hours. That way your body is getting a steady, regular supply of glucose with fewer ups and downs. And eating more often allows you to be satisfied with smaller meals and low-calorie snacks.
A good routine can help you stay on track. Try to eat your meals and snacks around the same time every day as often as your schedule will allow.
Start your day with breakfast.
It doesn’t have to be anything fancy as you’ll see in the sample menu plan below.
Don’t skip meals. You may not feel hungry or you may think that you’re saving calories by skipping meals.
Don’t. Do. It.
Cutting back on breakfast or lunch can leave you feeling sluggish, confused, nervous. All signs of low blood sugar.
Have a bedtime snack.
Without a nighttime snack, the time between dinner and breakfast the next morning could be anywhere from 10 to 12 hours!
A condition called nocturnal hypoglycemia–low blood sugar while you’re sleeping–is also a concern.
A low-calorie, low-carbohydrate protein bedtime snack can help your blood sugar remain level overnight.
Then start again the next day…with a nourishing breakfast.
#2 Eat a Balanced Diet
A balanced diet helps keep your blood sugar in a healthy range.
No single food can give you all the vitamins and minerals you need for a healthy pregnancy.
A lean cut of meat can give you B-12 but not vitamin C and grapefruit can give you vitamin C but not B-12. Spinach is a good source of iron. While carrots are an excellent source of vitamin A.
Mix it up. Vary the foods you eat for optimum health.
Having variety in your meals will give you the best possible benefits from your food choices.
And variety makes your plate less boring, more colorful, more interesting.
Eat a variety of foods in their proper proportions.
Try the plating method. There are many available, but here’s one specific to your needs.
MyPlate for Gestational Diabetes was created by the California Department of Public Health.
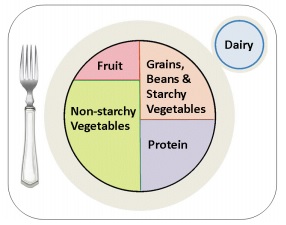 Fill nearly half your plate with non-starchy vegetables.
Fill nearly half your plate with non-starchy vegetables.
Then fill a quarter of the plate with a protein choice and the remaining portion grains, beans and starchy vegetables.
Reserve a small portion of your plate for fruit and a choice of dairy.
This built-in portion control can help create a healthy, balanced meal.
The Food Groups include:
- Starches
- Fruit
- Milk
- Non-Starchy Vegetables
- Meat and Meat Substitutes
- Fats
Some choices:
| Starches | Bread, Pasta, Oatmeal, Corn, Potato, Rice |
| Fruit | Pear, Mango, Raisins, Applesauce, Banana |
| Milk | 1% Milk, Soy Milk, Yogurt, Fat-Free Buttermilk |
| Non-Starchy Vegetables | Cabbage, Broccoli, Tomato, Beets, Green Beans |
| Meat and Meat Substitutes | Salmon, Beef, Egg, Tofu, Cheese, Baked Beans |
| Fats | Mayonnaise, Margarine, Corn Oil, Peanuts, Olives |
#3 Focus on Carbohydrates
Starches, fruit and milk. Those are your carbohydrate choices. Carbs for short.
Why are they so important?
Carbohydrates matter because they turn into sugar when we eat them. We need them for energy, but when you have diabetes, eating too many carbohydrates can increase blood sugar to the point where your body cannot process them correctly.
Counting carbs, like counting calories, can be tedious at times. Especially when you have to make note of everything that goes into your mouth. Instead try counting carbs per serving. That will make the counting process easier because you’ll be dealing with smaller numbers.
In addition to carbs, your health care professional may want you to be extra mindful of calories so that you gain an appropriate amount of weight over time.
So although calories are important, for now let’s focus on carbohydrates.
Here’s a quick overview of carb counting.
You can count carbs by the number of total carbs in the food you eat or by the number of servings. Counting the number of servings is much easier as you’ll see in the following example.
One serving of a carbohydrate-rich food contains about 15 grams of carbohydrates.
1 Serving = 15 Grams
Each of the following example servings have about 15 grams of carbohydrates.
STARCHES
1 slice of bread
1 corn tortilla
1/2 cup oatmeal
6 saltine crackers
FRUITS
1 small apple
12 cherries
1/2 grapefruit
1 cup papaya
DAIRY AND NON-DAIRY MILK
1 cup 1% milk
2 cups soy milk (unflavored/unsweetened)
1 cup plain yogurt or 1/3 c. fruit yogurt
Basic Carb Table – 15g per servings
| Breakfast (15g) | 1 Serving |
| Mid-Morning Snack (15g) | 1 Serving |
| Lunch (60g) | 4 Servings |
| Mid-Afternoon Snack (15g) | 1 Serving |
| Dinner (60g) | 4 Servings |
| Before-Bed Snack (15g) | 1 Serving |
| Total Carbs, 180 | Total Servings 12 |
Counting 12 servings is a much faster calculation than counting total carbs. Although counting actual carbohydrates will give you greater accuracy.
Of course, there are apps available that will keep track of carbs for you. I use Calorie Counter and Diet Tracker by MyFitnessPal. It has a food search database and also uses my phone’s camera for product barcode scanning.
There are many others apps available to help you track your carbs and other nutrients, but it’s still important for you to have a basic knowledge of carb counting principles.
Tracking recipes with multiple ingredients can be tricky.
Also foods loaded with sugar and flour will have a lot more than 15 grams of carbs per serving. For example, one cookie may be considered a single serving, but could have 40 carbohydrate grams in a single cookie.
Remember: Read labels carefully and check them for total carbohydrates per serving.
The basic carb table gives you something to work with and gives you a goal or direction for the day.
Your personal dietitian may have a different goal in mind for you. Instead of one serving of carbs at breakfast, she may want you to have two servings. Or instead of 4 servings at lunch, maybe 3 servings instead.
The above example is a basic table you can use to create a day’s menu.
Here’s a sample menu to help bring all the techniques together.
So here goes.
Using the Basic Carb Table as a guide, you might plan the following menu:
SAMPLE MEAL PLAN
BREAKFAST
- 1/2 cup oatmeal, cooked, made with water
- 1 egg, scrambled with 1 teaspoon vegetable oil
- coffee or tea, unsweetened
MID-MORNING SNACK
- bagel, 1/4 (1 oz)
- cream cheese, 1 tablespoon
- turkey, thin-sliced deli meat, 1 oz
- baby carrots, 1 cup
LUNCH
- 1 tortilla (flour or corn)
- ground beef, 1 oz
- shredded cheese, 1 oz
- taco sauce, 1 tablespoon
- lettuce and tomato
- salsa, 1/4 cup
- papaya, cubed, 1 cup
- 1% milk, 1 cup
MID-AFTERNOON SNACK
- vegetables, raw (broccoli, cauliflower, carrots) 1 or 2 cups
- salad dressing, reduced-fat, 2 tablespoons
- 1 boiled egg
- 1 packet sugar-free hot cocoa mix and water
DINNER
- baked chicken, skinless, 2 oz
- chicken broth
- onions, mushrooms, green peppers
- rice, 2/3 cup
- strawberries, 1 1/4 cup
- yogurt, plain, non-fat, 8 oz
BEFORE-BED SNACK
- 6 saltine crackers
- peanut butter, 1 tablespoon
Helpful Hints
- Avoid having fruit, yogurt or milk with breakfast. They tend to raise the blood sugar too quickly.
- Choose only one serving of fruit, milk or yogurt at lunch or dinner.
- Include protein and carbohydrates at each meal or snack.
- Protein and fats provide essential nutrients for your baby’s development, so eating them in moderation is good during pregnancy.
- Choose healthy fats like olive or canola oil, low-fat salad dressing or nuts.
- Protein does not contain carbohydrates and will help you feel fuller without spiking your blood sugar.
- Non-starchy vegetables like lettuce, carrots and broccoli are so low in carbs and high in nutritional value that their carbs are often considered “free.”
- Choose whole grains. They digest slowly and help you feel fuller longer and they keep blood sugar and insulin levels stable.
#4 Avoid Concentrated Sweets
Ahhh, the sweet tooth.
Candies, cookies, cakes. Jellies and jam.
You want ’em. You can’t resist ’em. They taste sooo good.
But they digest quickly, releasing glucose into your bloodstream, raising your blood sugar. And on top of that, they provide little to no nutritional value.
Concentrated sweets are high-sugar foods.
You can add fruit and milk to that list. And even though they contain vitamins, fiber and calcium; important nutrients and healthy sources of carbohydrates…as mentioned before, because they can raise blood sugar levels too quickly, they should be avoided at breakfast and consumed later in the day.
What to do?
- Choose fruit instead of fruit juice.
- Choose water or sugar-free drinks and avoid sugary soft drinks.
- Limit sugar-filled desserts such as cakes, cookies, and ice cream.
#5 Drink Lots of Water
You’ve heard it before. Water is important to your health.
But sometimes we still don’t drink enough of it.
Why is it so important?
Water helps our bodies function properly. Our blood circulation, digestion, body temperature – all depend on an adequate amount of water.
During pregnancy, water helps nutrients flow from mother to baby.
And we lose a lot of water everyday through urine, stool, sweat, even breathing. So we need to replace it.
Getting adequate water helps reduce the risk of urinary tract infections and kidney stones.
Chose water or caffeine-free, sugar-free beverages. If you drink caffeinated beverages, limit them to 200 mg of caffeine per day, about 1 1/2 8-oz cups of coffee. Studies have not conclusively shown that caffeine is harmful to unborn babies, but most authorities caution limited intake.
Are you having trouble reaching your quota of water? Try one or more of these strategies.
- Have a beverage with every snack and meal
- Keep track of your fluid intake as part of your meal plan
- Try adding a cup of low-sodium soup or broth to your meal
- Carry bottled water with you or stash it in your purse
- Keep a bottle of water or other beverage at your desk at work or near you at home
If these guidelines are new to you, then choose just one guideline. Read it over and begin implementing it today.
And work on it everyday until you’re ready to try another, then another, until they are second nature to you.
You may have to tweak them so that they better fit your personal needs, but you’ll be making strides in the right direction.
Practice makes progress.
